Episode Summary
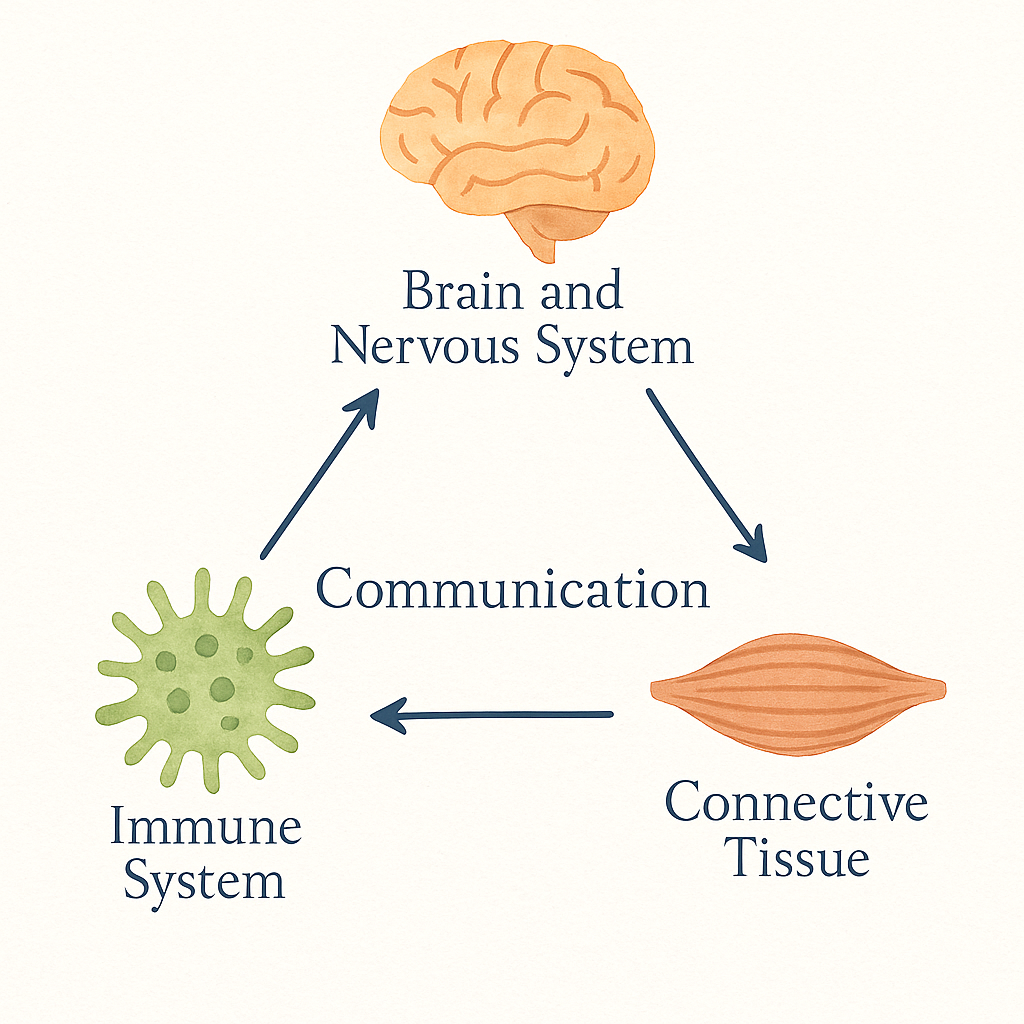
We’ve been told hypermobility is all about bendy joints — but what if that’s only part of the story? In this episode, we go beyond joints to explore how hypermobile Ehlers-Danlos Syndrome affects the entire body through connective tissue, the nervous system, and the immune system.
We’ll talk about how these systems “miscommunicate,” why symptoms can show up everywhere from digestion to fatigue, and how understanding this connection changes how we support our bodies.
It’s part science, part validation, and all about finally seeing your bendy body as connected, not broken.
Show Notes
In This Episode:
- Why hEDS is more than loose joints
- The three systems driving symptoms: connective tissue, nervous, and immune
- How miscommunication between these systems creates chronic inflammation and fatigue
- Why your body isn’t overreacting — it’s overprotecting
- Practical ways to support system regulation through nutrition and lifestyle
Resources Mentioned:
- Download the hEDS Living Guide
- Branch Collective Wellness/start — learn how foundational nutrition can support nervous system regulation
- Instagram: @chronically_misunderstood_pod
Key Takeaway:
Your body isn’t failing — it’s trying to protect you. When we address communication between systems, not just symptoms, everything starts to make more sense.
Transcript
Hi again, my chronically misunderstood friends.
It’s a cozy, rainy day here in Southern California, and I had plans for a different episode this week — but there is some new science that I’m super excited to share with you, especially any listeners who are extra bendy.
At the end of last month, a new study preprint was published identifying some of the genes contributing to hypermobile Ehlers-Danlos Syndrome.
The preprint title is “Complex Genetics and Regulatory Drivers of Hypermobile Ehlers-Danlos Syndrome: Insights from Genome-Wide Association Study Meta-analysis.”
This is a preprint — not yet peer-reviewed — but it’s a real step forward in understanding hEDS biology.
Unlike other EDS types that have one known gene, hEDS appears to be polygenic — influenced by several small genetic changes that affect how the nervous, immune, and connective tissue systems communicate.
It isn’t diagnostic yet, but in the future it could inform better support and, down the road, potential biomarkers or treatments.
The new hEDS genetics study identified two key regions in our DNA — not single “hEDS genes,” but areas that seem to influence how our body’s systems communicate.
Within those regions, researchers highlighted three strong candidates:
ACKR3, which affects how nerves and immune cells talk to each other;
SLC39A13, a zinc transporter that helps build healthy connective tissue; and
PSMC3, which supports nerve and brain development.
These aren’t rare mutations like in other types of EDS — they’re more like small switches that shape how different systems work together.
It’s the first real genetic evidence showing that hEDS is a multi-system communication issue, not just a collagen problem.
This study confirms what so many of us have known all along — hypermobility isn’t just about flexible joints.
It’s about how connective tissue, the nervous system, and the immune system communicate, and what happens when those messages get distorted.
When those systems misfire, the body gets stuck in an overprotective loop.
It confirms that what many of us live every day — the fatigue, gut issues, temperature swings, and pain — are part of one interconnected story, not separate random problems.
I’m not a doctor, and nothing I share is medical advice,
but as a Functional Nutritional Therapy Practitioner, I look at how body systems talk to each other and how we can support the body systems to function better.
My goal today is to show you what this research means for you — and what you can start supporting right away in your daily life.
Before we dive into the science, I want you to be able to see it.
I created a free companion guide called “Your hEDS Living Guide.”
It takes the key findings from the study and turns them into simple information, helpful visuals, and simple action steps you can apply immediately.
If you’re a visual learner or like to take notes, you might want to grab that first — it’s linked right in the show notes.
With that in hand, let’s zoom out and look at what this research actually shows inside the body.
Our connective tissue — fascia, tendons, ligaments — is more than scaffolding.
It’s a sensory and signaling network.
It’s filled with nerve endings, immune cells, and chemical messengers that communicate constantly with the brain and the rest of the body.
It’s basically Wi-Fi for the body.
When the collagen structure is altered, the “signal strength” changes too.
Previous research has shown altered collagen architecture and increased mast-cell activity,
and this new study helps explain why —
it links those findings back to the genetic communication pathways that regulate these systems.
When that network is built differently — which is the case in people with hypermobility —
the messages traveling through it can get distorted, delayed, or amplified.
It’s like the body’s text messages are full of typos.
The information still gets sent, but the meaning is off, and that creates a ripple effect across every system.
That’s why you might see such a wide mix of symptoms — joint pain, dizziness, gut problems, skin sensitivity, anxiety, and more.
The signals aren’t syncing.
The research is showing that it’s not weakness — it’s miscommunication.
The result is what they describe as a neuroimmune loop — connective tissue instability triggers nerve activation, nerve signals stimulate mast cells, mast cells release inflammatory mediators, and the cycle keeps feeding itself.
That feedback cycle is why the experience feels whole-body, not localized.
So, hypermobility isn’t just structural laxity — it’s a body-wide feedback problem.
What this means is that hypermobility sits at the intersection of structure and signaling.
The body isn’t broken — it’s trying to keep you safe, but the communication lines are overloaded.
And if miscommunication is the problem,
our support plan has to target communication itself.
Here’s the part that excites me the most:
We can absolutely support better communication through nutrition and lifestyle — the things we can influence every day.
I think of it as three main pillars:
Nourish the messengers,
Regulate the wiring,
and Reduce overload.
When I read the data, I immediately thought: this is exactly what we see clinically —
and it perfectly fits into three core priorities.
Every dysfunction described in the study — nervous-system reactivity, mast-cell overactivation, connective-tissue fragility — ties back to one of three themes:
The messengers aren’t getting what they need.
The wiring is overstimulated.
The environment is too noisy for clear communication.
These are the three pillars of support.
If you’re following along with the guide, you’ll see several watercolor diagrams that map these relationships —
how the nervous, immune, and connective systems overlap,
how communication flows in loops,
and how the cycle of Regulate → Communicate → Repair → Rebuild unfolds.
As you listen, notice which pillar feels most relevant for your body today;
you don’t have to do all three at once.
Let’s start with the raw materials in Pillar 1 by nourishing the messengers.
The study identified abnormalities in fibroblast activity — the cells that build and maintain collagen.
These fibroblasts rely on nutrients like vitamin C, lysine, proline, zinc, and copper to form proper cross-links that give tissue stability.
Without those cofactors, the tissue literally can’t translate messages correctly.
Collagen stays fragile and prone to micro-tears, which keeps inflammation active.
Mast cells also depend on nutrients for regulation — particularly magnesium, vitamin B6, and vitamin C, which help stabilize their membranes and reduce histamine release.
So, nourishing the messengers means feeding the communication network.
Balanced blood sugar gives the brain and nerves stable fuel.
Minerals like sodium and potassium help nerves fire at the right intensity.
Collagen-building nutrients strengthen the fascia so that mechanical stress doesn’t constantly trigger immune alarms.
When you give the cells the raw materials they’re asking for, the internal conversation becomes clearer.
Once the chemistry is supported, we help the circuitry in Pillar 2 by regulating the wiring.
The study also highlighted significant autonomic dysfunction in hypermobility — meaning the sympathetic and parasympathetic branches of the nervous system are out of sync.
Many participants had reduced vagal tone, impaired blood-flow regulation, and heightened sympathetic reactivity.
Researchers noted that people with hypermobility often show exaggerated sympathetic responses — the “fight-or-flight” mode stays on too long.
That chronic activation keeps mast cells primed and blood vessels unstable.
This imbalance explains symptoms like dizziness, temperature intolerance, rapid heartbeat, and digestive fluctuations.
It’s not “anxiety” — it’s dysregulation.
By intentionally regulating the wiring, we help the body shift back toward parasympathetic calm —
the state where repair, digestion, and immune balance happen.
This is why gentle vagal stimulation, predictable daily routines, and restorative movement are not “extras” —
they’re direct therapy for an over-signaling network.
Every cue of safety you give your body helps recalibrate the autonomic system.
Regulating the wiring starts with building predictability and safety signals:
- Gentle vagal stimulation through humming, slow exhalation, or devices like Pulsetto
- Consistent meal timing and sleep routines to anchor the nervous system
- Gentle strength work or water-based movement to retrain blood-flow responses
Each of these habits retrains your body to shift out of survival mode and back into repair mode.
If POTS-type symptoms are loud, it can be worth asking your practitioner about autonomic testing or additional support strategies.
Then we turn down the background noise in Pillar 3 by reducing overload.
Researchers found that nerve fibers in connective tissue had enhanced expression of pain and stretch receptors (TRPV1 and mechanoreceptors) — meaning the threshold for sensory input is lower.
Your body isn’t overreacting; it’s overreceiving.
Reducing overload allows your system to filter what truly matters and creates space for the body to process signals accurately.
Think of it as lowering the volume so you can hear the message.
Identify environmental or food triggers that keep mast cells activated (histamine, mold, chemical fragrances).
Simplify sensory input when possible — dim lights, consistent temperature, quiet spaces.
Build recovery moments throughout the day instead of waiting until burnout hits.
This isn’t avoidance; it’s nervous-system hygiene.
You’re teaching your body what “safe” feels like.
It’s also emotional — setting boundaries, saying no without guilt, and allowing your body to rest when it needs to.
Reducing overload is not weakness — it’s maintenance for a sensitive system.
When you:
Feed the tissue — the biochemistry,
Regulate the nervous system — the neurophysiology, and
Simplify the input — the environment and behavior,
you’re not just managing symptoms — you’re recalibrating the body’s entire conversation network.
These three pillars aren’t random wellness tips — they mirror what the study revealed at a cellular level:
Connective-tissue nutrition restores the body’s hardware.
Nervous-system regulation recalibrates the software.
Reducing overload protects the bandwidth.
When we address all three, we’re teaching the body to speak clearly again.
Or as the researchers put it:
“The connective tissue serves as the medium through which physiological coherence is either maintained or lost.”
This study reminds us that complex conditions don’t require complicated solutions — they require coordinated ones.
Small daily steps in nourishment, rhythm, and rest truly can re-tune the system.
So when we put this all together, the takeaway is that hypermobility is not just about flexibility — it’s about feedback.
When we support the way the body sends and receives messages, the entire system becomes more coordinated.
That’s why you might notice improvements in digestion, sleep, and focus, not just joint pain.
Everything is connected through communication.
This study confirms what many of us have felt all along:
Our bodies aren’t failing — they’re overloaded, trying to manage too much information.
And when we give them structure, nutrients, and calm, they finally start to make sense again.
If you want to see these connections and work through the steps to support your system, download the free guide Your hEDS Living Guide.
It walks through the study highlights, shows each diagram, and includes prompts to help you notice which communication systems in your own body might need the most support.
Bring the guide to your next appointment if you want shared language with your provider.
You can find it through the link in the show notes, on Instagram at Chronically Misunderstood Pod, or at BranchCollectiveWellness.com/start.
And if you know someone struggling with symptoms that never seem to make sense together —
share this episode with them.
Remember — your body isn’t failing. It’s communicating.
The more we listen, the more we learn what it needs.
Thanks for listening, friends — and next time, we’re talking about why fall flare-ups happen and how to get ahead of them before the season really hits.

Recent Comments